New Grant Enables Johns Hopkins Researchers to Implement Community Health Worker-Led Health Interventions for Noncommunicable Diseases in Nepal

Researchers at the Johns Hopkins Bloomberg School of Public Health received a new $3 million grant from the National Heart, Lung, and Blood Institute of the NIH to implement evidence-based interventions addressing risk factors of cardiovascular diseases by mobilizing community health workers in Pokhara Metropolitan City, the second largest city in Nepal. Researchers will be working in collaboration with the Nepal Development Society, an NGO based in Nepal.
The five-year grant, called Scaling Up Community-based Noncommunicable Diseases Research into Practice in Pokhara Metropolitan City of Nepal (SCALE-NCD), was launched in March 2024 and is led by Dinesh Neupane, PhD, MSc, assistant scientist and Yoko Inagaki, MD, MPH ’22, assistant scientist in the Department of International Health at the Bloomberg School.
Mortality from noncommunicable diseases, such as heart disease, diabetes, and cancer, is increasing around the world, with a disproportionate burden occurring in low- and middle-income countries. Three major risk factors for NCDs include high blood pressure, high blood glucose, and smoking. The health care system in Nepal, which suffers from a shortage of physicians and nurses, lacks a scalable and sustainable model to address these major risk factors for NCDs at the community level.
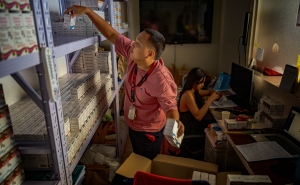
The goal of SCALE-NCD is to scale up evidence-based interventions for sharing clinical tasks with community health workers to fill the health worker void in helping to manage hypertension and diabetes and promote smoking cessation in an urban, LMIC setting.
“Community health workers are considered a backbone of the health system in many countries and historically have played an important role in reducing maternal, child, and infectious disease-related mortalities, particularly in rural areas. This project will allow us to evaluate female community health volunteers’ emerging roles on NCD management in urban settings of Nepal,” says Neupane.
Although trials led by Neupane and colleagues have documented that task-sharing with community health workers reduces blood pressure, blood glucose, and achieves smoking cessation, they are far from being fully implemented in routine health care delivery systems in LMICs, including Nepal. This project will provide evidence for scaling up a community-based intervention in which CHWs will conduct home visits, screen for blood pressure and diabetes, assess smoking status, refer individuals to health facilities for treatment, and provide counseling on smoking cessation and other lifestyle modification and medication adherence.
“This implementation research study will help us identify key factors to make the community health worker-led intervention equitable, cost-effective, and sustainable. We will have stakeholder engagement throughout the research lifecycle, which we hope can enable our intervention to be optimized and sustainable to urban health systems in LMICs,” says Inagaki.