Keys to the Navajo Nation’s COVID-19 Vaccination Success
Respect for community and elders, along with tribal sovereignty, equal strong COVID-19 vaccine uptake.

In early January, Laura Hammitt, MD, infectious diseases program director with the Bloomberg School’s Center for American Indian Health, set out from her Durango, Colorado, home to the Center’s Shiprock, New Mexico, office on the Navajo Nation to help with the reservation’s first COVID-19 mass vaccination event.
Approaching town, she saw a line of cars pulled off to the side of the road.
“I realized that these cars were lined up for two miles before the vaccine event was scheduled to start, and tears just filled my eyes,” Hammitt said. “This is a community that had suffered so much loss. And the vaccine offered hope, a way forward out of this pandemic.”
As of August 2, the CDC reports that the Indian Health Service has administered 1,497,047 vaccine doses, with 71,879 shots given daily per 100,000 of the total population in IHS jurisdictions.
The successful vaccine uptake follows a painful year in which Native communities saw some of the pandemic’s highest rates of illness and death. A key to the widespread vaccine acceptance is a community-centered culture.
“It’s embedded in our values that we don’t just think about ourselves,” says the Center’s Leonela Nelson, a research program supervisor with the Center’s Shiprock office, who lives in Arizona and belongs to the Navajo Nation. “We think about others and the generations that are going to come after us, so getting the vaccine is just one small thing that we’re able to do to ensure that life goes on.”
In this Q&A, Center director Allison Barlow, Hammitt, and Nelson reflect on how the COVID-19 vaccines brought much-needed hope to tribal communities.
What accounts for the successful vaccine uptake in many tribal communities?
AB: Several agencies across the U.S., as well as our Center and tribal leaders, made really important advocacy moves to promote vaccines getting to tribal communities when they were [granted] Emergency Use Authorization. And because some tribes participated in the vaccine trials, I think there was a building of information that the vaccines have been tested in tribal communities and they were working.
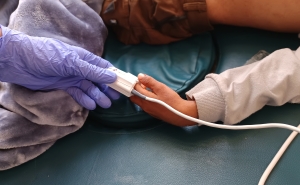
We also began to see the incredible strength of tribal sovereignty. The tribes are sovereign nations within the borders of states, and can enact their own policies for how vaccines will be distributed. They used a lot of creative methods to get vaccines out to their communities that included everything from vaccine blitzes to door-to-door campaigns. Indian Health Service teams embedded with folks from our Center’s community health representatives, and would literally go door to door with mobile units for the required vaccine storage and provide shots.
How did tribal values and culture contribute to vaccine acceptance?
AB: I think my [Center] colleague Victoria O’Keefe said it best. She really attributes what happened to a value system that favors community well-being and community responsibility over individual rights.
And I think there were three key influencing channels. There was a lot of focus on the elders and what our ancestors did to get us here, and it’s now our responsibility to carry on, and the way we do that is to protect all of the community. There were also a lot of youth-led campaigns, with the youth saying we need to protect our elders. In tribal communities, both elders and youth are viewed as sacred. The youth are the future, and elders are the keepers of the past and keepers of the codes, the culture, and traditions. The third was having Native American doctors and nurses speak out with their expert knowledge.
How did the vaccine campaigns overcome longstanding distrust of the U.S. government?
LH: Tribal communities have every reason to mistrust the government and government-backed efforts because of past atrocities. And while there is a long history of mistrust, we do have good levels of vaccine confidence in general in Native communities, and before the pandemic we’ve seen over many years high pediatric and adult vaccination rates. People know the reality of infectious diseases, and that leads them to value the protection that vaccines can provide. And IHS and tribal health programs have really done an excellent job with outreach and education about vaccines to help promote good vaccine uptake.
Some tribal communities around the country also made the decision to offer the choice of participating in COVID-19 vaccine clinical trials. So information about the vaccines was shared very early on at community meetings throughout the fall and the winter and really helped to provide a foundation for equitable access and confidence in vaccines. Also, there are many examples of tribal leaders and of native physicians being the first to roll up their sleeves and express confidence in the science and their belief in the importance of these vaccines to fight the pandemic.
Liana, can you describe how you persuaded a vaccine-hesitant relative to change his mind?
LN: We were a birthday party for my dad two months ago, the first family get-together in more than a year. A nephew of mine wasn’t vaccinated, and he was saying we really don’t know what’s going to happen in terms of vaccine side effects. I told him that we’re actually doing another family get together in a couple of weeks and that he couldn’t come because there will be other elders there and without being vaccinated, he would be risking everyone’s safety. And that did it.
The pandemic brought to light underfunded health care systems in Native American communities. Are there any planned improvements?
AB: In the spring, the American Recovery Act allocated the most funding ever to the Indian Health Service and to infrastructure support for tribal communities. What people don’t realize is the treaties that were signed with Native Americans in exchange for land promised them health and education for free in perpetuity. Those systems have never been funded adequately to deliver quality health and education. So there’s so much catch up, not to mention things like roads, water infrastructure, food, security, and so many other things that hopefully these new funds will support.
Jackie Powder is an assistant editor in the Communication & Marketing Office at the Johns Hopkins Bloomberg School of Public Health.