Why the FDA’s Approval of Opill Matters—And What’s Next
The decision could make oral contraception far more accessible—but it’s just one piece of a larger conversation.

Fifty years ago, the oral contraceptive medication norgestrel was FDA-approved for prescription use. Today, the FDA approved Opill, a brand-name version of this drug, for over-the-counter sale—giving millions of people access to safe, effective oral contraceptives at retail stores and online without a prescription.
The decision comes at a time when nearly half of pregnancies in the U.S. are unintended and abortion has been restricted or banned in many states.
In this Q&A, Carolyn Sufrin, MD, PhD, an associate professor of Gynecology and Obstetrics at the Johns Hopkins School of Medicine and in Health, Behavior and Society at the Bloomberg School, discusses the significance of Opill’s OTC availability, what needs to happen next, and why we should view this decision within a broader context.
Aside from this being the first approved over-the-counter daily oral contraceptive pill, why is this so important?
I'm thrilled about this because people with the capacity to be pregnant need to be able to decide and control if, when, and how they become pregnant and parent, and this is an essential tool to help many people determine that. Not having to go through a physician or other clinician reduces barriers to accessing effective pregnancy prevention.
One reason it's especially important now is that having an unplanned, unintended pregnancy in many states in this country can be a dangerous and difficult proposition because abortion is functionally unavailable in so many states. So if someone does not want to be pregnant and does not want to be a parent, they need to have access to contraception. This just makes it much easier for people to access a safe method of contraception.
Are there any caveats to the FDA’s approval?
Yes. I'm concerned about the cost and insurance complexities. It's great that it's going to be over the counter, but that doesn't mean that everyone's going to be able to afford it. I don't know what the cost will be—I hope they will make it affordable—but for someone who has limited income, it may be hard to purchase an over-the-counter medication.
Insurance companies may or may not cover this drug. The Affordable Care Act does require insurers to cover prescribed contraceptives, but it does not currently require coverage for over-the-counter medications. So I think that's going to be a tricky thing. I believe that the Biden administration has made a recommendation to HHS that they cover contraceptives, whether prescribed or not, but it's only a recommendation.
The promise of reducing barriers and promoting equity and access needs to be realized by making the medication affordable and by requiring insurers to cover it.
Do you have any concern about there being only one oral contraceptive option available?
There are two classes of oral contraceptive pills: One contains both estrogen and progestin, and one contains just progestin. The one that was approved for over-the-counter sale just has progestin.
Both pills are very, very safe—safer than many other over-the-counter medications—and have a long track record. There are a few more medical contraindications for estrogen-containing medications. For example, in some people with certain risk factors, estrogen can increase the risk of developing a blood clot in the venous system. It can [also] increase some people's risks of cardiovascular conditions or stroke.
For progestin-only contraceptives, there are few medical contraindications and very few safety concerns, and it's very easy for people to self-screen with the assistance of the pharmacist or online decision tools. Progestins are safer even than Tylenol, which has been available over the counter for a very long time.
I think there's a future for over-the-counter status for contraceptives with estrogen, but that requires just a little more complexity in terms of the screening safety and counseling on risks.
Now that Opill is approved for OTC sale, what needs to happen next?
Most immediately I want to see this become accessible for people for the cost reasons we discussed. I also think we need mobilization and partnership from our pharmacy colleagues. We need a lot of education and a lot of support from pharmacists, because people might come to them with questions, and we want to make sure that pharmacists are able to provide nonbiased, accurate support as well as referral information when people need it. Some people may need education on using the medication as well as support if they want to use something that does require a prescription.
In the long term, we still need comprehensive policies and procedures in place to increase access to a range of contraceptive methods. That may include advocating for over-the-counter status for combined oral contraceptive pills just to increase the options. It may also mean reducing barriers to people accessing injectable contraception. There's a version of Depo-Provera [the contraceptive injection] that people can self-administer, so I think efforts to expand that availability over the counter is also a next step.
Importantly, [this discussion] is not just about contraception. We can't think of this in isolation. We have to support people with having access to quality prenatal care as well as abortion access, and we know that's not happening comprehensively and equitably across our country.
Are you concerned that there could be backlash to this decision?
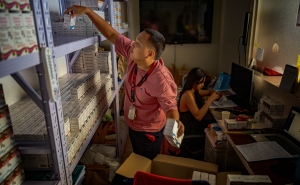
I am concerned that organizations that oppose this very safe and effective medication are going to respond by demanding that laws be passed that allow pharmacists or pharmacies to object to stocking their shelves with this medication. We saw a version of this with mifepristone, which pharmacies can provide without a physician or clinician directly administering it. I'm concerned about state laws that could put up all kinds of barriers to making this a reality. We also could see laws at the federal level with a different administration. So, I am concerned about availability.
It's great that FDA has authorized this, but that's only one piece of this puzzle.
Melissa Hartman is the managing editor of Hopkins Bloomberg Public Health magazine and associate director of editorial at the Johns Hopkins Bloomberg School of Public Health.