New Study Highlights Link Between Minimum Wage, Income Inequality, and Obesity Rates Across U.S. Counties
Research represents a significant step forward in understanding the complex relationships between economic policy, place, and health.

A new study published in the Journal of Racial and Ethnic Health Disparities in October reveals a significant interaction between minimum wage policy, income inequality, and obesity rates in U.S. counties. The research conducted by a multidisciplinary team of Department of Health Policy and Management researchers led by Hossein Zare, PhD, underscores how factors such as income inequality, state-level minimum wages, access to healthy food, and racial/ethnic composition shape obesity outcomes, particularly in economically and racially segregated communities.
The study analyzed data for 3,129 U.S. counties and county equivalents between 2015 and 2019, using the County Health Rankings for obesity rates-defined as measured by BMI ≥30 kg/m²-and socioeconomic variables from the American Community Survey, which included the Gini coefficient, a well-known measure of income inequality. The analysis revealed that counties with state minimum wages between $7.26–$9 saw a reduction in obesity by 0.6 percentage points, while counties with minimum wages over $9 experienced an obesity reduction of 2.8 percentage points.
There was also a positive association between income inequality and the obesity ratio. Counties with higher Gini coefficients, indicative of greater income inequality, had significantly higher obesity rates. This relationship persisted even after controlling for variables such as age, gender, and racial/ethnic composition.
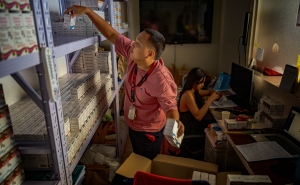
In addition to the minimum wage policy, the study examined the role of access to healthy foods in shaping obesity outcomes. Counties with lower access to healthy food—measured by a composite Food Environment Index (FEI)—had higher obesity ratios. The correlation between poor food environments and obesity was especially pronounced in racially segregated counties, where communities faced greater barriers to accessing affordable, nutritious foods.
The study also explored the interaction between racial/ethnic composition at the county level and obesity. Black and Hispanic adults, who experience some of the highest obesity rates in the U.S. (49.9% and 45.6%, respectively), are disproportionately affected by both income inequality and poor food environments. The study found that counties with higher concentrations of Black and Hispanic populations saw even sharper increases in obesity as income inequality rose, particularly in areas with low access to healthy food.
"Income inequality isn’t just a social or economic issue; it’s a public health issue," Zare said. "When wealth is unevenly distributed, disadvantaged populations often lack access to essential resources, including healthy food options, which puts them at greater risk for obesity and related chronic conditions. The data suggest that when individuals have more income, they are better able to make healthier lifestyle choices, which can ultimately reduce obesity rates."
The study’s authors argue that the findings have significant implications for both policymakers and public health professionals. Minimum wage increases, combined with efforts to improve access to healthy foods, could serve as effective interventions to reduce obesity rates, particularly in low-income and minority communities. The authors also call for place-based interventions that address the specific needs of these communities, such as urban farming initiatives, subsidies for healthy food retailers, and community nutrition programs.
"Addressing obesity is not just about encouraging individual behavior change," Zare emphasized. "It’s about creating environments where healthy choices are the easy choices. Economic and social policies, like raising the minimum wage and improving food access, are essential to creating those environments."
While the study offers valuable insights into the relationship between minimum wage policy, income inequality, and obesity, the authors acknowledge the need for further research. They suggest longitudinal studies to assess the long-term impact of minimum wage increases on health outcomes and suggest incorporating individual-level data on socioeconomic status and health behaviors to provide a more comprehensive understanding.