What You Need to Know About the Johnson & Johnson Vaccine

The FDA confirmed Emergency Use Authorization after reviewing the safety and efficacy of Johnson & Johnson’s vaccine. Here’s what you need to know.
By Lindsay Smith Rogers, Reviewed by BY Joshua Sharfstein and Andrew Pekosz
It’s a different kind of COVID-19 vaccine.
The Johnson & Johnson vaccine is a nonreplicating viral vector vaccine, a method with decades of research behind it. This vaccine uses adenovirus, a common cold virus that, when modified, is able to enter cells but can’t make new virus particles. Researchers add the gene for the coronavirus spike protein—the protein on the surface of SARS-CoV-2—to this modified adenovirus. When injected into a person’s arm, the adenovirus carries this genetic material into human cells and trains the immune system to react against the coronavirus.
That’s why it’s more durable and requires just one dose.
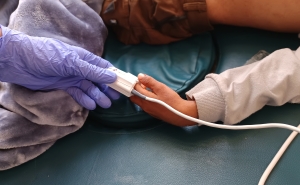
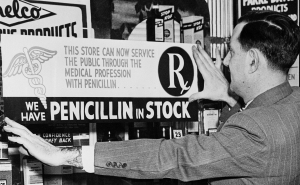
Unlike mRNA vaccines, which must be stored at -20 degrees C, adenovirus vaccines can be refrigerated for up to three months at 36–46 degrees F. That means it can be distributed more easily in doctor’s offices, pharmacies, clinics, or anywhere else. This vaccine promotes a robust immune response after just one dose.
The J&J vaccine is 66% effective while the Pfizer and Moderna shots are as high as 95% effective. It’s important to keep two things in mind.
- The J&J vaccine appears to be even more effective against serious illness than it is against moderate COVID-19. The flu vaccine, which prevents hundreds of thousands of deaths and serious illnesses every year, is about 40%–60% effective. When COVID-19 vaccines were being developed, it was hoped that they would be at least 50% effective. Pfizer’s and Moderna’s vaccines vastly exceeded all expectations for a good working vaccine, and the J&J also appears to be quite effective.
- Some people may prefer the one-shot regimen of the J&J vaccine, given the high levels of protection against serious illness. This vaccine provides a substantial amount of protection against COVID-19, is safe, and its broad use will hasten the decline in COVID cases. That’s why many public health departments will use it with multiple populations to be vaccinated.
SOURCES: STAT, The New York Times, CDC, and Politico
Joshua Sharfstein, MD, is the vice dean for Public Health Practice and Community Engagement and a professor in Health Policy and Management. He is also the director of the Bloomberg American Health Initiative and a host of the Public Health On Call podcast.
Andrew Pekosz, PhD, is a professor in Molecular Microbiology and Immunology with a joint appointment in Environmental Health and Engineering.
Lindsay Smith Rogers is the producer of the Public Health On Call podcast and the associate director of content strategy for the Johns Hopkins Bloomberg School of Public Health.
RELATED CONTENT
More from the Bloomberg School
- See latest headlines
- Learn more about our departments: