What We Know About Rwanda’s Marburg Virus Outbreak
How Rwanda is working to contain the deadly virus—including by testing a new vaccine.

Late last month, Rwanda reported its first-ever case of Marburg virus disease. Like Ebola, Marburg can cause severe hemorrhagic fever and has high case fatality rates (20% to 90%, depending on the strain).
The virus spreads from fruit bats to humans, who can then transmit the virus to other humans. There are currently no approved treatments or vaccines for Marburg, though testing is underway.
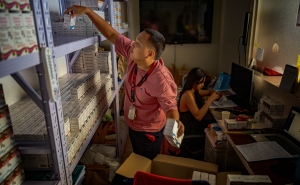
As of October 15, Rwanda has confirmed 62 Marburg cases—80% of which were among health care workers—and 15 deaths. The outbreak has so far been contained to Rwanda, and the risk to the public in the U.S. is low.
In this Q&A, adapted from the October 15 episode of Public Health On Call, virologist Kari Debbink, PhD, MEd, an associate teaching professor in Molecular Microbiology and Immunology, gives an overview of Marburg virus, the state of the outbreak in Rwanda, and why we’re seeing more cases of zoonotic diseases like Marburg.
What is Marburg virus?
Most people may not know about Marburg, but they’ve probably heard of Ebola. These are similar viruses in terms of the symptoms that they cause and their mortality rates. These viruses kill a large number of the people they infect, usually through hemorrhagic fever: The virus destroys the blood vessels, causing bleeding from many different places.
Where does the outbreak in Rwanda stand, and what are people concerned about?
As of October 5, there were 46 confirmed cases and 12 deaths, with the majority of those being health care workers. [Ed. note: Rwanda regularly updates its website on the topic.] And as you can imagine, if health care workers are getting infected, it weakens the area’s overall health infrastructure, which is a major problem. Right now, case numbers are still going up. Hopefully, now that there’s more international focus on this and attention, we’ll start to see those numbers go down as there’s more aid and more care taken to identify cases and contain them.
Hospitals and health care facilities must be on high alert, knowing that anybody could come in with this virus.
Yes. A lot of times what happens with Marburg or Ebola is that the first case happens in more rural areas, because that is where contact with an infected animal would occur. Then the virus spreads from person to person from that original contact.
When people come to the hospital, the hospital workers don’t know if it’s a Marburg case. In the early days of a Marburg case, it can mimic other types of infectious diseases. You may not know it’s something as serious as Marburg until it’s had time to infect health care workers.
Now that there is a known outbreak, certainly people are taking higher precautions with anyone who comes in with symptoms consistent with a Marburg infection.
Ebola spread widely in the last decade. Are there concerns that this could become another Ebola?
There’s always concern that a virus can spread, but in this outbreak, the cases were confirmed before it had spread to multiple areas. The biggest Ebola outbreak that we had, back around 2014, happened because it spread so far before it was really known what it was. When we did know, multiple countries were involved and it was really hard to contain cases.
This Marburg outbreak has really been contained to Rwanda. I think there’s a pretty low risk for it to spread as widely as Ebola did in 2014.
We’re also seeing a lot of testing for Marburg. Is this a new development?
We now have a lot more testing available for many diseases than we ever have in the past. We can do PCR testing for Marburg, which is the best way to confirm that you actually have a specific virus, and that’s available in most major cities. There are also blood tests for viral proteins and antibodies. So yes, I think the testing infrastructure is better than it has been in the past, for Marburg and other pathogens as well.
There’s no approved vaccine for Marburg, but there is an experimental vaccine being sent to Rwanda. Can you tell us about that?
The Sabin Vaccine Institute sent about 700 doses of this experimental vaccine to Rwanda. It’s going to be used primarily in health care workers, to protect them and hopefully prevent spread to other people as well. [Ed. note: The Sabin Vaccine Institute has since supplied an additional 1,000 vaccines.]
The vaccine is based on the Marburg glycoprotein—the part of the virus that sticks to cells and helps the virus enter. The vaccine then induces your body to generate antibodies against the part of the virus that allows it to infect cells. It has already been tested for safety in Uganda and Kenya, two countries that have previously seen Marburg outbreaks. That first-line testing showed it was safe and wasn’t causing major side effects, so now they feel safe sending it to health care workers in Rwanda.
This may allow them to get data on how well the vaccine protects against Marburg. For a lot of rare diseases where there are smaller outbreaks and then the virus goes away for a while, it’s hard to do the testing necessary to show protection. The best way to do that testing is to vaccinate people during an outbreak of the disease and see how well the vaccine protects them. So this is a way to both protect health care workers and hopefully get a vaccine one step closer to being licensed.
This is what happened with the Ebola vaccine during the 2014 outbreak. Before that, there was not good enough data on how well the vaccine protected. They did what is called ring vaccination, where anybody who had been in contact with an infected person was vaccinated. Then, over the course of the outbreak, they could see how many vaccinated people got Ebola and how many people didn’t and could basically estimate an effectiveness, and it was very successful for Ebola.
Has Marburg virus been around for a long time?
We don’t know how long it’s been around, necessarily. But the first cases were identified in 1967, in labs in Germany and the former Yugoslavia, where monkeys had been imported from Uganda to use in research. Some people working with those monkeys got infected with Marburg, and that was how it was identified. We don’t know how long it’s been circulating in the countries where it’s endemic, but that was the first time the virus was characterized.
It seems we’re hearing about more and more of these diseases that spread from animals to humans. Why is that?
There are a few reasons. First of all, we live in a much more global society than we ever did. There’s more travel—people travel all over the world, live all over the world, have family all over the world. People in the U.S. might not have thought or heard much about diseases like these because we didn’t see them here, but now we hear about them more because people think they could impact us in some way.
People are also having more contact with animals that carry these pathogens. As we develop land, we’re moving closer to their habitats and encountering these animals more than we used to. Marburg virus is transmitted by the Egyptian fruit bat. Most people may not be out in caves where they’ll encounter a fruit bat, but people who do work in mining, for example, may be exposed to these bats or their feces, urine, or saliva. The bats may also feed on fruit that humans eat, which could have deposits of urine, saliva, or feces on them. And people travel more between rural areas, and between rural and more populated areas, so there’s a greater chance that diseases that were once isolated to small areas can spread to larger population centers.
This interview was edited for length and clarity by Melissa Hartman.