What to Know About Ketamine
The anesthetic is being used off-label for everything from psychiatric illnesses to autoimmune diseases.

After the death of actor Matthew Perry, ketamine—for decades used as a popular party drug—came into the public eye once more. According to the medical examiner, Perry, who had been undergoing “ketamine infusion therapy” for depression, had levels of the drug in his body in the range used for general anesthesia during surgery.
While the actor’s death wasn’t shown to be directly connected to his therapy, it did call into question how ketamine—which is not FDA-approved for the treatment of mental health disorders, much less Lyme disease, alcoholism, or other ailments for which it’s been advertised as a cure—is being used today.
In this Q&A, adapted from the January 26 episode of Public Health On Call, Lindsay Smith Rogers speaks with Caleb Alexander, MD, MS, professor of Epidemiology and co-director of the Center for Drug Safety and Effectiveness, about the drug’s dangerous side effects and addictive potential, and how antiquated marketing laws allow its promotion for unproven uses.
What is ketamine?
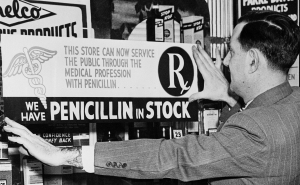
Ketamine is an NMDA receptor antagonist, meaning it blocks the N-methyl-D-aspartate neurotransmitter in the brain. It was developed in the 1960s and used as a battlefield anesthetic in the Vietnam War, as well as clinically in health care settings. But the settings in which ketamine was developed and historically used were highly regulated and supervised inpatient health care facilities. That’s not how ketamine is being used in 2024.
Is ketamine approved for mental health treatment?
There's one other actor in this play that’s important to mention, which is esketamine. Ketamine and esketamine are chemically very similar, but they're two different drugs. Ketamine is only FDA-approved as an anesthetic, and is still widely used for anesthesia and acute pain in surgical, operative, and emergency trauma settings. Esketamine was brought to market around 2019 for the management of treatment-refractory depression [depression not responsive to standard treatment]. Most of what we're hearing about in the news is ketamine.
More from Public Health On Call: Ketamine and Esketamine
How is ketamine being used “off label”?
Thanks to an interesting loophole in the laws governing drug advertising, ketamine is now marketed for the management of any number of different psychiatric illnesses. Depression, anxiety, post-traumatic stress disorder, and chronic pain are the big ones, but it's also being marketed for other uses, ranging from Lyme disease to alcoholism to opioid addiction. As is often the case, enthusiasm and marketing have gotten ahead of the evidence.
Just because a product is marketed for a use does not mean it’s approved for that use—is that correct?
Typically, drug companies are restricted to marketing and promoting their products only for FDA-approved indications. But in the case of ketamine, the product is being marketed and promoted by clinics and telehealth companies that aren't manufacturing the drug.
The laws and regulations that govern drug marketing and promotion are enforced by the overlapping authorities of the FDA and the Federal Trade Commission and a patchwork of state consumer protection statutes. But they were written in an era before the rise of telemedicine and pop-up clinics. If you look at the claims being made by these entities regarding the safety and effectiveness of ketamine, they range from potentially misconstruing the evidence to being bald-faced lies.
Is ketamine safe and effective for treating mental health issues?
One of the pearls of the field of pharmacoepidemiology is that it's not just about safety or effectiveness, it's about safety and effectiveness and the balance of these.
With ketamine, we have a drug that has unclear effectiveness with some very well described dose-response and cumulative adverse effects that run all the way up to death. There is a remarkable dearth of evidence of well controlled, randomized, blinded trials, which really represent the gold standard for how we assess effectiveness. Many trials only look at short-term, not at moderate or long-term, outcomes of effectiveness. And the measures of effectiveness are often quite limited.
Safety is really where things open up, because this is a drug that affects perception and can cause hallucinations and visions. It can cause mood changes, ranging from euphoria to suicidality. It affects behavior, ranging from sedation to violence. And it typically reduces cognition. The biggest concern is that the effects aren't always short-lived and the onset of these effects isn't always immediate.
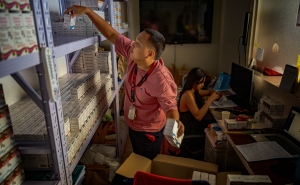
In these instances, how is ketamine being administered?
This is a drug that should be administered in highly controlled, highly supervised, structured clinical settings. But it's being used in a lot of different settings, the most concerning of which is non-health care settings. In some places, you can get this drug compounded by a pharmacy for in-home use, which is really asking for trouble. The drug is also being used and delivered in cash-only clinics. These clinics can purchase a vial for less than $100 and charge $500 to $1,500 for an infusion. Insurance may not cover it. The non-anesthesia uses aren't FDA-approved; these are off-label uses. It's a cash business.
Drug compounding adds extra uncertainty into the mix. These compounds are loosely regulated, and the notion that you would use this as a nasal spray or something is just bonkers. Having any standardization of the exposure is very difficult when you're compounding. You can’t really control the dose that you receive.
Read more: Esketamine for Treatment-Resistant Depression (Johns Hopkins Medicine)
Is ketamine addictive?
I don't think we have the same level of evidence that we do with opioids, where we have many well-designed, rigorously developed studies, but there is a risk of addiction.
Given the marketing loopholes, is there any impetus to do efficacy research for these indications?
Unfortunately, you have a drug that's available for more or less pennies, and there really is not the incentive for manufacturers to go out and do these studies, to say nothing of the challenges of doing the studies and doing them well. Even the FDA’s approval of esketamine was fairly controversial.
We need to modernize and revise the laws and rules governing pharmaceutical marketing and promotion so that they constrain the behavior of companies that currently are making outlandish claims about ketamine’s safety and effectiveness.
Is there interest in exploring esketamine as a treatment for some of these conditions as opposed to using ketamine?
I don't know the degree to which esketamine is currently under serious clinical investigation for some of these other psychiatric indications. It would stand to reason that the manufacturer would have an enormous incentive to identify and get FDA approval for other indications. PTSD, or possibly severe generalized anxiety disorder, might fit that bill.
What are some of the risks of self-medicating with this drug?
Ketamine has been a party drug for decades. It was developed only after its earlier cousin, PCP, was abandoned because of the dissociative properties and the violence and aggression associated with its use and potency.
Self-medication is risky. Millions of Americans are self medicating with alcohol, and others increasingly with marijuana, and so on, all the time. I certainly think clinicians and patients should be talking about these things. But the bottom line is, ketamine is a very, very dangerous drug. Anybody self medicating with this is taking some pretty big risks.
Lindsay Smith Rogers, MA, is the producer of the Public Health On Call podcast, an editor for Expert Insights, and the director of content strategy for the Johns Hopkins Bloomberg School of Public Health.