6 Things to Know About the Microbiome and Your Health

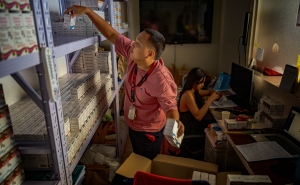
Jotham Suez and PhD candidate Annie Gao quantify bacteriophages.
Jotham Suez has a tough job.
He studies the microbiome—the universe of bacteria, viruses, fungi, and other microbes that each of us is home to. In sheer numbers, there are as many of them as there are human cells in the body.
“We’re studying the whole complexity of the human body. We’re also studying the complexity of billions of microbes of hundreds of different species—each one of them with their own genes and their own proteins,” says Suez, PhD, MSc, an assistant professor in the W. Harry Feinstone Department of Molecular Microbiology and Immunology.
Why study the bugs in our gut, on our skin, behind our ears? Because science is increasingly revealing the massive influence they have on our health.
Below, Suez shares six things you need to know about the microbiome.
1. Your microbiome is like a biological fingerprint.
The collection of bacteria, viruses, and other bugs you have is unique to you. Researchers swabbed computer keyboards in an office for microbes and then swabbed fingertips of workers for a 2010 study. Then they were able to determine which keyboard was used by which person. These person-to-person differences in the microbes that we host can affect everything from our responses to diets and drugs, to disease risk, and even our behavior—they’re as important to our health as our own genes.
2. You have more than one microbiome.
Microbes find multiple ecological niches in and on your body. Your skin microbiome is distinct from your gut microbiome or oral microbiome. Each one has adapted to the conditions there, such as the lack of nutrients on the skin, the moisture or dryness of different areas of the armpit, or the acidity in the vagina.
In fact, while at the Weizmann Institute of Science in Israel, Suez worked with gastroenterology colleagues to sample from 18 different sites along the upper and lower gastrointestinal tract of 46 people. In two papers in the journal Cell (here and here), he found that each site had its own unique microbiome signature.
“When we're trying to understand the mechanisms of how microbes cause disease or promote health, we need to make sure that we’re looking in the right place,” says Suez. “For example, if you’re interested in interactions between the microbiome and the immune system, you might learn more from studying the microbes in the small intestine, rather than the ones washed out in stool samples.”
3. Ask your microbiome what’s the best diet for you.
Dietary advice is often based on the food’s calories or carbohydrate content rather than who eats the food. It assumes, for example, that if two people ate identical pieces of bread, the changes in the blood glucose would be roughly the same.
Not so.
Suez and his colleagues found that blood glucose levels spiked in some people but didn’t budge in others. In fact, they measured widely different glucose responses to any given food. The takeaway is that the same food or diet can be healthy for some but unhealthy for others.
Based on data collected from hundreds of participants, Suez and colleagues developed an algorithm that could predict glucose responses based on the microbiome alone. In follow up studies by his collaborators, the algorithm was able to recommend a diet that was healthier for individuals with type 1 diabetes or prediabetes than a traditional diet that excluded high-carbohydrate foods like bread altogether.
4. Your medications may soon be changed based on your microbiome.
Doctors typically prescribe the same drug to everyone with the same condition. But not all drugs work equally well for everyone. For example, University of Washington researchers recently found that the effectiveness of statins (medications that lower cholesterol levels) varies depending on the person’s microbiome.
Another striking example: The microbiome underlies responsiveness to cancer immunotherapy, according to three studies published back-to-back in Science in 2018.
Advanced genetic sequencing of microbiomes will allow researchers to understand which drugs are effective in which people. That will allow them to create algorithms that help predict which person would respond to the drug and which person wouldn’t. This would replace doctors arbitrarily giving the same drug to everyone and then seeing if it works. These algorithms could also help minimize side effects.
5. Probiotics won’t necessarily improve your health—or your microbiome.
If you look at whether probiotics are effective in treating a condition like gastroenteritis, the answers will be all over the place. Some people respond to probiotics, and some do not. To learn more, Suez and his colleagues gave 10 healthy individuals probiotics and then examined their fecal samples. Everyone had lots of the probiotic bacteria in the samples. But samples from participants’ intestinal tracts revealed that some people had huge numbers of these bacteria, while they weren’t even present in others.
Basically, the study found the microbiome either allowed the probiotics to thrive, or it rejected them.
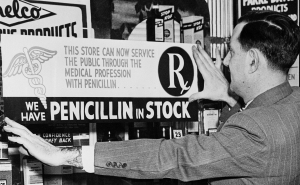
Probiotics are often recommended for people who have taken antibiotics; the idea is that they help rebuild bacteria in the gut that have been wiped out by the drugs. However, in a separate study, Suez and his colleagues were surprised to discover that in some cases, probiotics can delay, rather than enhance, the microbiome’s post-antibiotic recovery. Considering the importance of the microbiome to our health, its delayed recovery may increase an individual’s risk to various diseases, although according to Suez, more research is needed. Interestingly, Suez and his colleagues recently reported that following antibiotics, probiotics increased the number of antibiotic-resistance genes in the gut.
This could be an important and under-explored contributor to the spread of antibiotic-resistant infections, which pose a major global health threat. But Suez says it’s premature to provide advice on taking probiotics with antibiotics and advises patients to consult with their doctors. Notably, the American College for Gastroenterology has recently published revised guidelines that recommend against the use of probiotics with antibiotics in the treatment of C. difficile infections.
6. Noncaloric artificial sweeteners may damage your microbiome–and your health.
Seeking to lose weight, many people use sugar substitutes. But Suez says using them isn’t a good idea—because they can change some people’s microbiome and elevate blood glucose, which can lead to weight gain and type 2 diabetes, as revealed in his newest study published in Cell. Although, in some people, the same sweeteners had no effect.
“What we're trying to do now here at the Bloomberg School is understand how sweeteners can negatively impact the microbiome and metabolic health,” says Suez. By doing that, he hopes to identify the pathways involved so that future diagnostics can determine which people can safely use sweeteners—and which people need to seek out alternatives.
Brian W. Simpson is the editorial director at the Bloomberg School.