Chagas: The Most Neglected of Neglected Tropical Diseases
The disease is treatable if caught early, but on-the-ground surveillance is thin.
On a research trip to Bolivia about four years ago, Robert Gilman visited a Chagas patient at San Juan Dios Hospital in Santa Cruz de la Sierra, the country’s largest city.
“I walk into the room and they show me a chest X-ray. His heart was literally the size of a basketball,” says Gilman, who travels to South America six times per year to study Chagas disease in its most endemic region.
At just 45 years old, the man was almost certain to go on to die of heart failure. Tragically, that’s how it often goes with Chagas disease.
The man had likely been infected with Chagas as a child via the bite of a “kissing bug” but was never diagnosed. Then the disease lay dormant, causing no symptoms for decades until the telltale signs emerged: fatigue; swelling of the legs; then an inability to sleep lying down or walk; and later, being almost entirely confined to bed.
This is the fate of an estimated 30% of Chagas patients whose disease progresses to debilitating heart failure. Most don’t even know they have the disease until it’s too late for existing treatments to be effective.
While devastating, “it’s not uncommon,” says Gilman, MD, a professor in International Health at the Bloomberg School and of medicine at the Johns Hopkins School of Medicine who has studied Chagas for 15 years.
Yet global Chagas surveillance is patchy at best, meaning a similar fate awaits thousands of children infected every year in utero or while growing up in the poor, rural areas where the vector thrives.
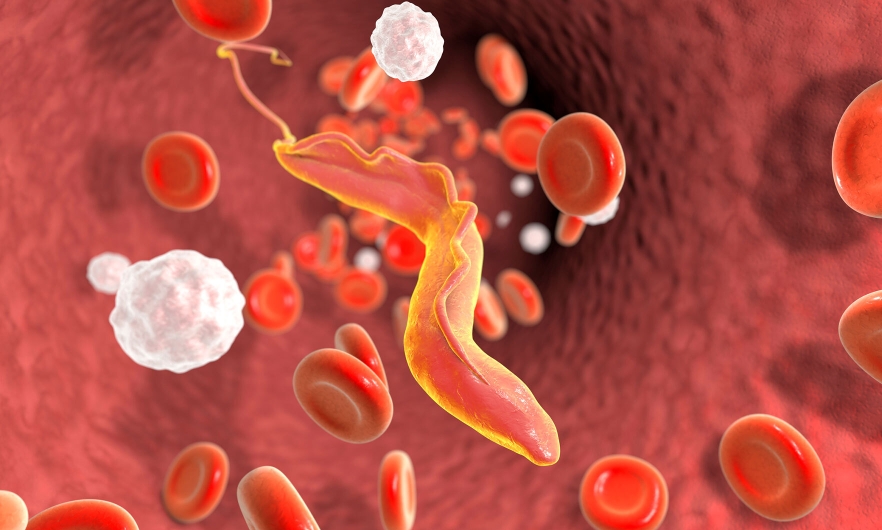
Trypanosoma cruzi, the parasite that causes Chagas, is most often transmitted by the blood-sucking triatomine bug. These “kissing bugs” live primarily in the walls or roof cracks of structures like adobe huts and chicken coops in South America, Central America, and Mexico. They feed on people’s exposed skin at night, spreading the parasite through bug feces that enter broken skin or the eyes or mouth. Transmission is also possible through contaminated food.
While most Chagas patients are infected as children, the disease’s most devastating effects manifest in middle-aged or older individuals whose illness has become chronic.
Chagas causes inflammation of the heart that can affect how it beats, which can cause sudden death. It can restrict blood flow from the heart, leading to congestive heart failure. It can also cause serious digestive issues.
An estimated 6–7 million people worldwide are infected with T. cruzi. About 10,000 deaths every year result from Chagas—the bulk of them are in poor communities of Central and South America.
But rising migration is expanding Chagas’ footprint to non-endemic areas including the U.S. and Europe where, even in the absence of kissing bugs, Chagas can still spread from infected mothers to their babies in utero, as well as through blood transfusions and organ donation.
Chronic underfunding for research has hobbled efforts to improve surveillance and vector control and to update archaic diagnostics and treatment. An estimated 90% of global Chagas cases go undetected—and Gilman suspects the real figure is considerably higher.
A key problem is that existing testing protocols are, in a word, “crappy,” says Gilman.
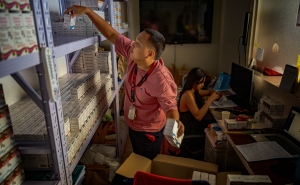
For one, existing serological tests may be reliable for detecting strains that circulate in the most endemic countries like Bolivia, but not for the variant circulating in, say, Mexico and El Salvador. Existing PCR tests work well for flagging congenital infection but not for identifying decades-old infection in adults. At-home rapid tests haven’t hit the market, so diagnostics require skilled technicians.
And crucially, “in most of the world, most people never get a test at all,” says Gilman.
That’s particularly frustrating because, while there’s no vaccine for Chagas, the disease is “brilliantly treatable” in young children if it’s caught and treated promptly, says Gilman. But only an estimated 1% of patients receive available treatments.
The two go-to Chagas therapeutics—the antiparasitics benznidazole or nifurtimox—are nearly 100% effective in curing the disease if given to children soon after infection.
When it comes to treating Chagas, that’s where the scientific consensus ends, says Gilman.
Treatment protocols remain highly controversial and their effectiveness for chronic disease remains in doubt.
One thing that’s clear is that for adults with chronic disease, these drugs can trigger debilitating side effects that lead many patients to abandon treatment early. Up to 40% of treated adults experience adverse reactions that can range from nausea to insomnia to anxiety and depression. Treatment takes up to two months and requires regular monitoring.
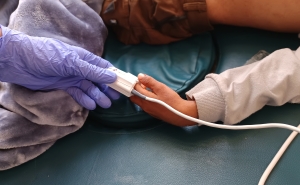
But there’s a glimmer of hope, says Gilman: Those side effects have not been seen in babies who’ve been treated for the disease—meaning this bleak trajectory can be stopped by screening pregnant people so their newborns can be promptly treated.
“The problem is that there’s no widespread program to roll that out,” says Gilman.
Pockets of dedicated surveillance and treatment programs have been successful, but their reach is limited to areas where political will and funding exist.
The nonprofit Drugs for Neglected Diseases Initiative is funding a trial of rapid Chagas tests in Santiago del Estero, Argentina. In that province, all pregnant women are screened for the disease under the targeted initiative ‘Not a single baby with Chagas.’ In April 2021, the governments of Argentina and Brazil signed on to the initiative to eliminate mother-to-child Chagas transmission by 2030.
But such programs are the exception, not the rule, despite Chagas’ expanding footprint beyond South America.
The CDC estimates that 300,000 people in the U.S. are infected with T. cruzi. Without early treatment, a significant number of them will go on to Chagas-related cardiac disease, Gilman warns.
But U.S. Chagas surveillance remains thin and has been further back-burnered by the pandemic. In September 2021, the CDC paused testing for Chagas and other neglected tropical diseases, leading to an outcry from tropical disease researchers.
From 2009 to 2018, Chagas disease research received a global grand total of $236.31 million in funding—representing just 0.67% of the total applied for all neglected diseases during that period.
The National Institutes of Health covered more than half of that, but “a lot more—hundreds of millions of dollars more” is needed to improve and expand testing and physician knowledge, improve treatment, to roll out screening and treatment programs for congenital Chagas, and study the risk factors for severe disease, says Gilman.
And there’s little interest from Big Pharma. One study stated frankly that the pharmaceutical sector “does not have any serious interest in financing specific research against Chagas disease.”
And while it was certainly overshadowed by the pandemic, one step toward raising Chagas’ profile was WHO’s establishment of World Chagas Day in 2019, which came with a call for stepped-up government investment in surveillance, treatment, and breaking chains of transmission.
The theme for 2022: Finding and reporting every case.
Annalies Winny is the associate editor of Global Health NOW.