The New Technology Behind COVID-19 RNA Vaccines and What This Means for Future Outbreaks
How RNA Vaccines Will Provide Protection from the Virus
In this interview adapted from the December 3, episode of Public Health On Call, Stephanie Desmon talks to Johns Hopkins immunologist Diane Griffin, MD, PhD, about the development of RNA vaccines and how they will provide protection from the virus.
Could you tell us a little about what these RNA vaccines are, and why they’re so different from what we’ve seen in the past?
What we want to do with any vaccine is deliver the viral protein that you want the person being vaccinated to make an immune response to. There are lots of different ways to do that. One is to give the whole virus—inactivated, so it doesn’t make the person sick. Another way is to deliver the nucleic acid that encodes the protein, and let the [vaccinated person’s] cells actually make the protein.
RNA is the nucleic acid that codes for proteins that cells make. Basically, it has all the information needed to be able to synthesize the protein. The idea of these vaccines is that you deliver the RNA that encodes the viral protein you’re interested in, and let the cell actually make that protein and to then stimulate the immune system.
What are the benefits of this?
It has several advantages. Because the cell itself is going to make the protein, it’s much more likely to be the native protein, or have the right folding and energetic properties of the protein that the virus would also have. Another big advantage is that they’re fast to make. If you have the basic platform that [allows you] to insert the sequence for your particular protein of interest, you can just take [that] out and put another one in. It’s very fast to substitute in a new, different coding sequence for a protein.
Also, the manufacturing turns out to be relatively straightforward for these types of vaccines. You don’t have to grow them in cells or do a lot of things that either make manufacturing difficult or [require going] through a lot of hoops with the FDA to prove that your cells are not contaminated. It bypasses all those steps.
It has required a fair amount of manipulation of the RNA, because RNA intrinsically is unstable. These RNA vaccines have been engineered to make them somewhat less likely to be reactogenic, [or likely to] make you sick. The RNA also has to be put inside of something. What’s currently being used and has turned out to be most successful is what they call a lipid nanoparticle, which basically surrounds the RNA that’s going to be the vaccine and does two things: First, it protects the RNA from being degraded. Second, it interacts with cells [to allow the RNA to enter]. Then the RNA can be released for the cell to actually make the protein that you want.
These are the first RNA vaccines that have gotten this far in the process. I guess there was a lot of work done leading up to this moment that made it sort of the perfect moment to try these. Is that right?
That’s right. Probably for the last 10 years, people have been working on these kinds of vaccines.
There are two versions. The current two vaccines that we’re dealing with [use] just the messenger RNA. There’s also a version [that uses] a self-replicating RNA, where it also has the information needed to copy that RNA, so you make more copies of it. They’ve been worked on mostly for cancer vaccines. Both self-replicating and non-self-replicating RNA have been explored for quite a period of time for immunization purposes as well.
Why were we able to adapt it for the virus that causes COVID-19 when they couldn’t really get it into production for these other things they’ve tried?
They have had prototypes for influenza, for rabies, for a number of other [viruses], but they’ve never gotten to phase 3 testing. I think maybe the need was not so emergent and so critical as it has been here. [COVID-19] has really motivated [researchers] to move the technology forward fast. But as you say, there’s really been a lot of work that’s been ongoing for the last five to 10 years with this platform.
What’s the potential going forward? Does this mean that we will be able to react quickly to things? Does this mean perhaps we could create a flu shot that’s more effective?
I think that we’re very likely to see other vaccines [using this platform]. [SARS-CoV-2] came along as a brand-new virus, so it opened the way to apply these newer methods. I think there are still questions about how durable this immunity is, but yes, I think it’s likely to get applied to more emerging infectious. Where we have other new viruses coming on the scene, it may embolden people somewhat to try it. And there is work using this platform for influenza vaccines as well.
Are these generating stronger immune responses than traditional vaccines?
I think they’re good immune responses, but I don’t think they’re necessarily better. I think we’ve just been happy that they were good.
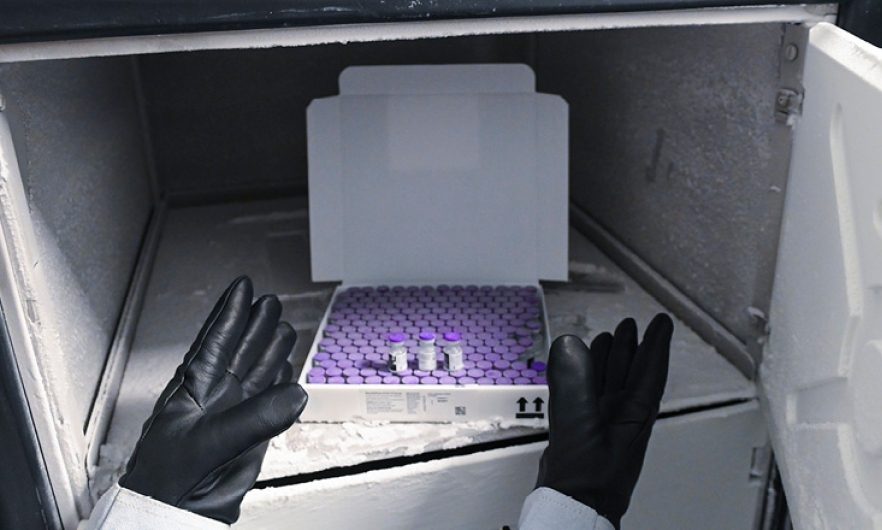
The Pfizer vaccine needs to be stored at -70 degrees Celsius, and the Moderna vaccine needs to be stored at -20 degrees Celsius. Do these vaccines need to be kept cold because of the RNA?
Yes. RNA is unstable at higher temperatures. I think that the Pfizer vaccine can withstand a little bit warmer than -70, but it hasn’t been tested or proven. Drug companies need to be able to say that they left the vaccine at whatever temperature for two weeks and tested it. I think it’s probably been easiest to say, “We know it’s OK at this really low temperature, so that’s what we’re going to use.”
For practical reasons, it feels like there’s some urgency for Pfizer to find that it can be held not quite that cold.
Yes, I would imagine. I don’t have any inside information that they’re working on that. Because the Moderna vaccine can be stored at a higher temperature—or a more reasonable available temperature—[it would seem] that Pfizer will be investigating that possibility for their vaccine, as well.
Not only was this developed quickly, it seems like it can be manufactured more quickly.
Well, it doesn’t require eggs, and it doesn’t require cells. It just requires ingredients that you mix together in the manufacturing facility. These vaccines have never been manufactured before at large quantities, and scaling up is not always as straightforward as just doubling the recipe. So, I think that that is still an issue. But the manufacturing facilities anticipated the success of the vaccines, and I think both companies have invested in manufacturing facilities, and even manufactured the vaccine in advance of getting the data from their trials.
You’ve been doing this a long time. You must be really excited to see a whole new category of vaccine to come out.
I’ve been interested in this technology. We work on measles, and we worked on some of the prototype self-replicating vaccines for measles in monkeys. We never brought it as far as testing it in people, but they work very well.
Diane Edmund Griffin, MD, PhD, is a professor in the Department of Molecular Microbiology and Immunology at the Johns Hopkins Bloomberg School of Public Health.
RELATED CONTENT
Public Health On Call
This conversation is excerpted from the December 3 episode of Public Health On Call.
