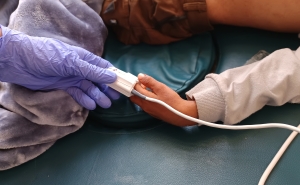
Back to School: Vaccinating Kids and Teens
COVID-19 shots have been available to kids 12 and up since early March, and as of August 15, more than 10 million children under age 18 have received at least one dose.

As we look ahead to making the vaccines available to children 12 and younger, Stephanie Desmon discusses the benefits of vaccinating kids, whether it should be mandatory for attending school, and how it can help end the pandemic with Kawsar Talaat, MD, an associate professor in International Health and co-director of clinical research at the Johns Hopkins Institute for Vaccine Safety, and Odis Johnson Jr., PhD, a Bloomberg Distinguished Professor with appointments at the Bloomberg School and the Johns Hopkins School of Education.
At the moment, nobody younger than 12 can be vaccinated. When is that going to change?
KT: I can’t predict when the vaccines will be available for children under 12, but I know that both Pfizer and Moderna are doing clinical trials right now in that age group in the United States. We’re hoping to have some data in the fall.
But the determination will be left up to the FDA, which decides whether a vaccine is granted emergency use authorization in that population or if they are going to wait for the full set of data and go through the licensure process, which will take a lot longer. They are thinking about this, and we’ll see what they do when the data is available.
Many companies are now making the COVID vaccine mandatory for their employees. Do you think that will happen for kids going back to school?
OJ: Well, we just established that for many kids—those under 12—this is not even going to be possible. For those over 12, we should strive to get as many of them as possible vaccinated, but I don’t know that school systems can be in the business of mandating a COVID-19 vaccine in particular. And I don’t think it’s possible, primarily because states vary so much in their approach to COVID. In those states with governors who are less worried about COVID, I don’t know that even corporations will actually take that approach.
In order to go to school, my kids needed their measles shots, their tetanus shots, I think even the new meningitis shot that my son just got. Those are required for school. Why is the COVID vaccine different?
OJ: I think we’re in a new era when it comes to vaccinations. We saw this coming years ago, when vaccines became politicized. Now we’ve gotten to a very contentious political climate and I doubt there’s going to be the ground support—meaning families and communities that would go along with a mandatory COVID-19 vaccinations. Despite the epidemiological or health data out there—science that actually says that it’s safe and that it’s to everyone’s benefit—there has to be political will to put this public health approach in place, and it’s just not there.
There’s a school of thought that maybe we shouldn’t vaccinate kids until the rest of the world’s adults have been vaccinated. Where do you stand on that?
KT: I actually agree with that to a great extent. I vaccinated my teen because the vaccine is available here in the United States and I want to protect her and keep her safe. I’m happy that the vaccine is available for her and hopeful that it will be available for my younger child, but I also wish that it was available for my family and colleagues in other countries, who are much older and at much higher risk.
We know that the people who are most vulnerable to COVID are people who are older and people with preexisting conditions. If we’re trying to save the most lives, we want to vaccinate as many people as possible who are at the highest risk, no matter where they live. If we’re talking about stopping the transmission of COVID, then we want to vaccinate as many people as possible, no matter what the age and no matter where they live.
As long as there are people who are unvaccinated where the virus can spread, we can have new variants that are more contagious, potentially more deadly, and that may escape from the vaccines we have now. So the most important thing is to vaccinate as many people as possible everywhere in the world. But I would prioritize those who are at the highest risk of severe illness and death.
We’re seeing the kids become a larger proportion of those who get sick. Is that a concern?
KT: There is a report from the CDC showing that between January and March, in 14 states the number of teenagers hospitalized with COVID has gone up. A third of them ended up in the ICU and 5% ended up intubated. So this is not a trivial disease, even in healthy teenagers.
OJ: A lot of those risk factors that we were talking about at the height of the COVID pandemic are also those that families should be worried about now: childhood obesity, asthma, diabetes—all of these factors increase the risk of hospitalization after infection. Yes, children are resilient, but at the same time, they can have the same conditions that make them more likely to be hospitalized, for the infection to be more serious.
Do you think parents with younger children are going to be more reluctant to get those children vaccinated?
OJ: I think the younger your child is, the greater concern you may have about their tolerance to the vaccine or their reaction to it. I’ve heard from families with really young kids saying, “We’re going to sit this one out” because they’re not certain what the reaction may be. I think they are going to be skeptical until it’s backed by lots of trials and science that says it’s safer for young kids.
Kawsar, you do this exact work for a living: You study vaccines in young children right now. Are there different checks in place for rolling those out?
KT: The FDA is looking very carefully at the safety of the vaccines in all populations, but especially as you go down in age, because the risk-benefit ratios change.
With people who are older, who are more at risk for severe disease or dying from COVID, you’re going to accept a little more risk with a vaccine than with somebody who is younger, who is less likely to have that. We’re looking very carefully at the safety of the vaccines in children, and the FDA has very strict criteria for what needs to be met in order to authorize the vaccine in younger age groups.
These vaccines have been rolled out very quickly, but they’ve been rolled out in millions of people. We know the safety profile really well in 200 to 300 million adults. And we know that children behave differently than adults, but that is a very reassuring safety profile.
Stephanie Desmon is the co-host of the Public Health on Call podcast. She is the director of public relations and marketing for the Johns Hopkins Center for Communication Programs, the largest center at the Bloomberg School of Public Health.
Public Health On Call
This conversation is excerpted from the July 7 episode of Public Health On Call.