How Nipah Virus Spreads From Person to Person
Largest-ever study of Nipah virus transmission concludes that older male patients and patients with respiratory problems are more likely to transmit infection to other people
The deadly Nipah virus, which is carried by bats and occasionally infects people, is more likely to be transmitted from person to person when the infected patient is older, male and/or has breathing difficulties, according to a study co-led by scientists at the Johns Hopkins Bloomberg School of Public Health.
The study, published May 9 in the New England Journal of Medicine, is, to date, the most comprehensive evaluation of person-to-person transmission during Nipah virus outbreaks. These outbreaks, all in Asia, have been relatively small to date, but the fatality rates at the outbreak level have been very high, ranging from 40 to 100 percent.
Epidemiologists fear that Nipah virus, a distant cousin of the measles virus, could mutate to become much more infectious among humans and cause a catastrophic pandemic. The findings suggest that reducing exposure to respiratory secretions from infected patients should be a priority in future outbreak responses.
“As health systems evolve and patients get more hands-on care from clinical staff and undergo more invasive procedures in places where Nipah virus outbreaks occur, there may be opportunities for wider transmission in hospitals,” says study co-senior author Emily Gurley, PhD, associate scientist in the Department of Epidemiology at the Bloomberg School. “By understanding the factors that influence transmission, we can reduce our future vulnerability to this dangerous pathogen.”
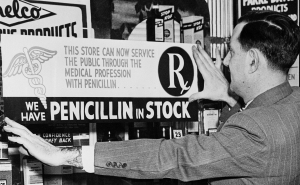
Nipah virus was first identified in 1999 following an outbreak in Malaysia that led to the deaths of more than 100 people in a pig-farming region and the culling of more than a million pigs from local farms. Nipah virus’ principal animal hosts are fruit bats that are found widely throughout much of the globe—from Australia, across tropical Asia and through to the east coast of Africa. But the virus sometimes spreads to pigs and other animals, as well as humans. Gurley was the senior author on a 2016 study that found bat-contaminated date palm sap was the most common source of human outbreaks in Bangladesh.
Nipah infection in humans causes fever and encephalitis, or brain inflammation, often with seizures and coma. Some patients also develop a pneumonia-like respiratory illness. In Bangladesh, where public health surveillance of Nipah virus outbreaks is more extensive than anywhere else, the case fatality rate is about 75 percent.
For the study, the research team, using datasets collected during routine surveillance and outbreak investigations in Bangladesh, analyzed all 248 cases of Nipah virus infection that were investigated in Bangladesh from April 2001 to April 2014. The 248 cases represented about 40 percent of the total Nipah virus cases reported in the medical literature. The aim was to identify factors associated with transmission of Nipah virus from one person to another.
The team concluded that only 82 of the 248 cases were likely to have been caused by transmission from another infected person; the rest were believed to involve animal-to-human transmission. The scientists sorted the 82 person-to-person cases into 17 “transmission trees” originating from animal-to-person cases. The largest of these mini-outbreaks included 32 cases. The vast majority (86 percent) of the 82 person-to-person transmissions were believed to have originated from just 12 patients.
The researchers’ analysis linked a few key factors to increased risk of person-to-person transmission of Nipah virus. One was gender: Male patients infected about eight times as many people as did female patients. Another was age: almost all the transmission events originated from patients older than 45 years. All of the “super-spreader” patients were older males.
The presence of respiratory illness was yet another risk factor: Virtually all the person-to-person transmissions came from infected patients who had breathing problems, which is consistent with the idea that the virus can travel in saliva and respiratory secretions, such as those expelled by coughing.
Finally, transmission appeared to occur during the acute, symptomatic phase of the illness, and the severity of illness was another factor in transmission risk. “All the patients who infected others were patients who later died of their own infection,” Gurley says.
Why men appear to be better transmitters of Nipah infection isn’t yet clear. “We thought that they might have more contacts, compared to women, but surprisingly we found that the average number of contacts didn’t really differ between Nipah patients who spread the disease and Nipah patients who didn’t,” Gurley says.
The team recommends that public health measures to prevent major Nipah virus outbreaks should focus on contacts of infected patients, and should include measures to limit exposures—among personal contacts and health care workers—to saliva and respiratory secretions from patients.
The study was co-led by Gurley, with colleagues at the International Centre for Diarrhoeal Disease Research, Bangladesh (icddr,b) and the Bangladesh government’s Institute of Epidemiology, Disease Control and Research, and the Centers for Disease Control and Prevention. Simon Cauchemez, PhD, from Institut Pasteur in France, co-led the analysis.
“Transmission of Nipah Virus—14 Years of Investigations in Bangladesh” was written by Birgit Nikolay, Henrik Salje, M. Jahangir Hossain, A.K.M. Dawlat Khan, Hossain M.S. Sazzad, Mahmudur Rahman, Peter Daszak, Ute Ströher, Juliet R.C. Pulliam, A. Marm Kilpatrick, Stuart T. Nichol, John D. Klena, Sharmin Sultana, Sayma Afroj, Stephen P. Luby, Simon Cauchemez, and Emily S. Gurley.
Support for the research was provided by the National Institutes of Health (2R01-TW005869); the Centers for Disease Control and Prevention; the National Institute of General Medical Sciences; the AXA Research Fund; the European Union; Institut Pasteur; and the governments of Bangladesh, Canada, Sweden, and the United Kingdom.
# # #
Media contacts for the Johns Hopkins Bloomberg School of Public Health: Jonathan Eichberger at 410-502-5494 or je@jhu.edu and Barbara Benham at 410-614-6029 or bbenham1@jhu.edu.